Example Article
Understanding Chikungunya Virus: Origins and Virology
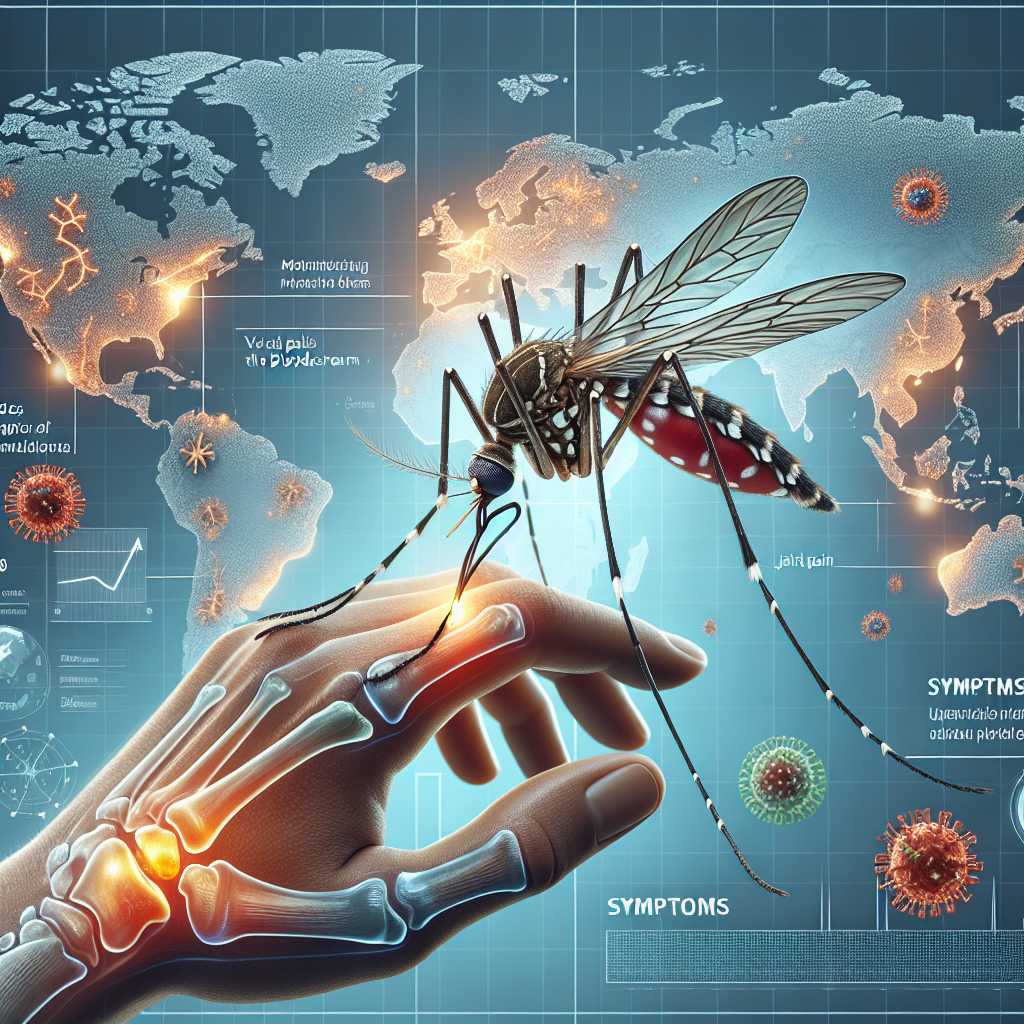
Chikungunya virus (CHIKV) is an arthropod-borne virus primarily transmitted to humans through the bite of infected Aedes mosquitoes, predominantly Aedes aegypti and Aedes albopictus. First identified in Tanzania in 1952, CHIKV has since evolved into a global health concern, with outbreaks documented across Africa, Asia, Europe, and the Americas. The virus belongs to the Alphavirus genus within the Togaviridae family, characterised by a positive-sense single-stranded RNA genome. This genetic structure allows rapid replication and adaptability, contributing to its capacity for outbreaks.
The name ‘chikungunya’ originates from the Makonde language, meaning "that which bends up," alluding to the characteristic joint pain that forces sufferers into a bent posture. The virus’s ability to cause debilitating arthralgia distinguishes it from other arboviruses such as dengue or Zika, although co-infections can occur. Molecular studies have revealed three main genotypes of CHIKV — West African, East/Central/South African (ECSA), and Asian — each with distinct epidemiological patterns and virulence factors.
Recent research has highlighted genetic mutations in the E1 envelope glycoprotein that enhance the virus’s transmission efficiency via Aedes albopictus mosquitoes, facilitating its spread into temperate regions previously considered low-risk. This evolutionary leap emphasises the importance of continuous genomic surveillance and vector control strategies tailored to regional mosquito populations.
Clinical Manifestations and Challenges in Diagnosis
The clinical presentation of chikungunya infection typically begins abruptly with high fever, severe polyarthralgia or polyarthritis, rash, myalgia, and headache. While symptoms generally resolve within one to two weeks, joint pain can persist for months or even years in some patients, mimicking chronic rheumatic diseases such as rheumatoid arthritis. This prolonged morbidity significantly impacts quality of life and poses challenges for healthcare providers in both diagnosis and management.
Diagnosing chikungunya can be complicated due to symptom overlap with other arboviral infections like dengue fever and Zika virus disease. Laboratory confirmation relies on molecular techniques such as reverse transcription-polymerase chain reaction (RT-PCR) during the acute phase or serological assays detecting IgM and IgG antibodies during convalescence. However, cross-reactivity among alphaviruses and flaviviruses may confound serodiagnosis.
Moreover, resource-limited settings where chikungunya is endemic often lack access to advanced diagnostic tools, resulting in underreporting and misdiagnosis. This diagnostic ambiguity underscores the necessity for improved point-of-care tests that are affordable, sensitive, and specific to facilitate timely intervention and epidemiological tracking.
Epidemiological Trends: The Expanding Footprint of Chikungunya
Over the past two decades, chikungunya has transitioned from a relatively obscure tropical illness to an emerging global health threat. The 2005-2006 epidemic on Reunion Island marked a turning point when over 300,000 people were infected, spotlighting its epidemic potential outside traditional African foci. Since then, large outbreaks have been reported in India, Southeast Asia, the Caribbean, South America, and even parts of southern Europe.
The expansion is driven by multiple factors including urbanisation, global travel, climate change, and widespread distribution of competent mosquito vectors. Warmer temperatures extend mosquito breeding seasons and geographical range while increased human mobility facilitates rapid dissemination of viraemic individuals into new areas.
Public health systems worldwide face significant challenges in controlling chikungunya outbreaks due to these multifaceted drivers. Surveillance systems must integrate entomological data with human case reports to predict risk zones effectively. Furthermore, international collaboration is critical for sharing outbreak data and deploying coordinated vector control measures.
Innovations in Prevention and Therapeutics: The Road Ahead
Currently, there are no licensed vaccines or specific antiviral treatments for chikungunya virus infection; management remains supportive focusing on symptom relief through analgesics and anti-inflammatory agents. However, recent advances in vaccine development offer promising prospects. Several candidates employing live-attenuated viruses, viral vectors, mRNA platforms, and virus-like particles are undergoing clinical trials with encouraging immunogenicity profiles.
Vector control remains the cornerstone of prevention strategies. Innovative approaches such as Wolbachia-infected mosquitoes that reduce vector competence or genetically modified sterile males are being trialled in endemic regions with some success. These biological methods complement conventional insecticide spraying and habitat reduction but require sustained community engagement.
Additionally, awareness campaigns educating at-risk populations about personal protective measures—such as use of insect repellents, window screens, and eliminating stagnant water—are vital components of integrated vector management programmes. Ultimately, combining vaccination with advanced vector control could transform chikungunya from an episodic epidemic into a manageable endemic disease.
Conclusion: Addressing Chikungunya’s Emerging Global Impact
Chikungunya virus exemplifies how arboviral diseases can rapidly evolve from localised tropical infections into pressing global health challenges fueled by environmental changes and human behaviour. Its capacity for causing prolonged joint disease imposes a hidden burden that extends beyond acute illness episodes.
To mitigate this threat effectively requires a multidisciplinary approach encompassing enhanced surveillance technologies, robust diagnostic capabilities accessible worldwide, innovative vector control solutions, and accelerated vaccine deployment once validated. Moreover, strengthening healthcare infrastructure in vulnerable regions will improve patient outcomes and outbreak responsiveness.
In summary, recognising chikungunya’s expanding footprint demands proactive investment in research and public health initiatives now—transforming scientific insight into tangible interventions that protect populations against this persistent viral adversary.
Notes
- Chikungunya outbreaks have affected millions globally since the early 2000s.
- The virus’s name reflects its hallmark symptom: severe joint pain causing a bent posture.
- Mutations enhancing transmission via Aedes albopictus have facilitated spread into temperate zones.
- No licensed vaccines exist yet but multiple candidates are advancing through clinical trials.