Example Article
Understanding Babesiosis: An Underappreciated Tick-Borne Illness
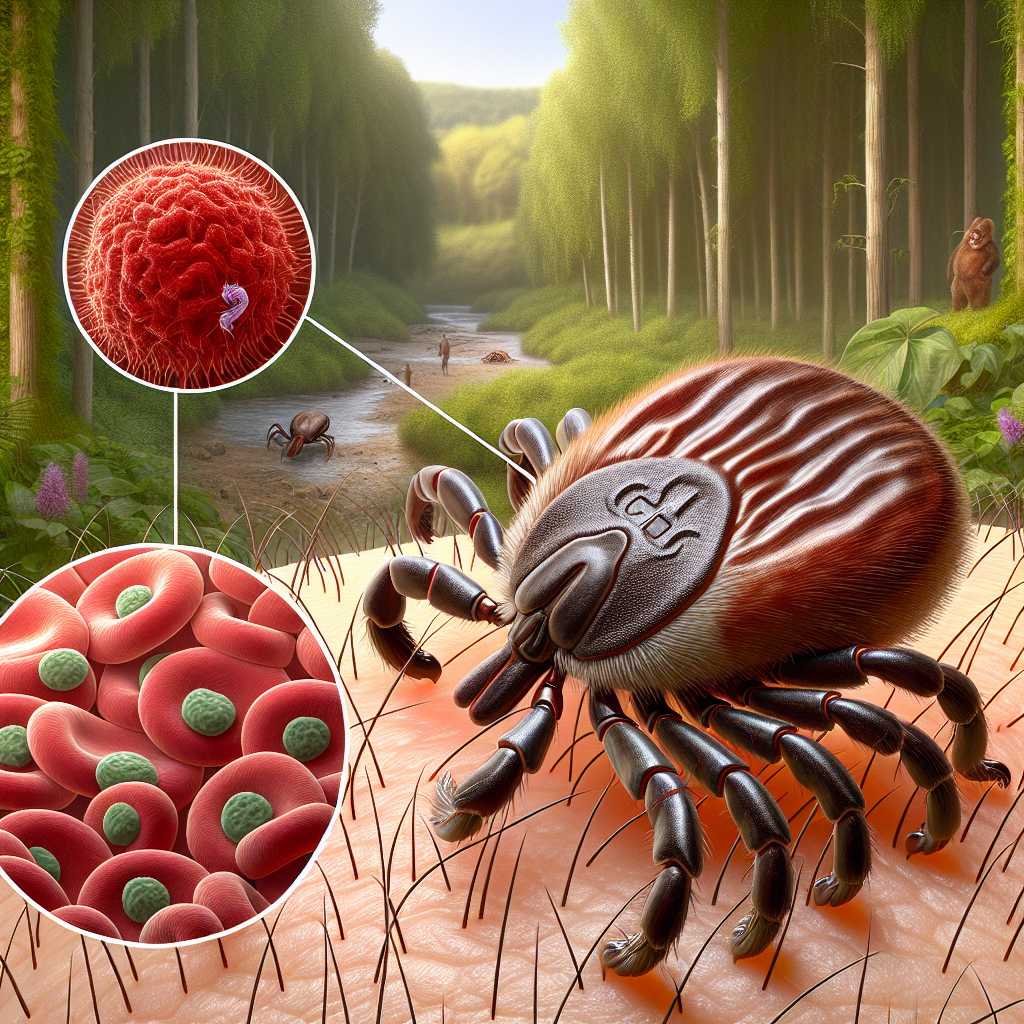
Babesiosis is a parasitic disease caused by microscopic protozoa of the genus Babesia, primarily Babesia microti in the United States and Babesia divergens in Europe. Transmitted through the bite of infected Ixodes ticks—the same vectors responsible for Lyme disease—Babesiosis affects red blood cells, leading to symptoms that can range from mild flu-like discomfort to severe haemolytic anaemia. Despite its clinical similarities to Lyme disease, Babesiosis remains less well-known among both the public and many healthcare professionals.
The disease’s pathology centres on the invasion and destruction of erythrocytes, which distinguishes it from Lyme disease, caused by the Borrelia burgdorferi bacterium. This difference means that diagnosis and treatment protocols vary significantly between the two diseases. Furthermore, co-infection with Lyme disease and Babesiosis is common due to shared tick vectors, complicating patient outcomes and therapeutic strategies.
Babesiosis has been reported predominantly in the Northeastern and upper Midwestern United States, but cases have emerged across Europe and Asia. The increase in tick populations due to climate change and expanding human encroachment into wooded areas suggests that Babesiosis may become a more pressing public health issue globally.
Clinical Features and Diagnosis: Navigating Overlapping Symptoms
The clinical presentation of Babesiosis often overlaps with other tick-borne illnesses, making accurate diagnosis challenging. Common symptoms include fever, chills, fatigue, muscle aches, and headaches. In severe cases, particularly among immunocompromised individuals or those without a spleen, patients may experience haemolytic anaemia, jaundice, respiratory distress, or organ failure.
Diagnosing Babesiosis requires a combination of clinical suspicion based on exposure history and laboratory testing. Microscopic examination of blood smears can reveal characteristic intraerythrocytic parasites resembling malaria parasites. However, this method requires expert interpretation and may miss low-level infections. More sensitive molecular techniques such as polymerase chain reaction (PCR) assays have improved diagnostic accuracy but are not universally available.
Serological tests detecting antibodies against Babesia species can support diagnosis but may not distinguish active infection from past exposure. Given these complexities, clinicians must maintain high vigilance for Babesiosis in endemic areas or when patients exhibit symptoms unresponsive to standard antibiotic regimens used for Lyme disease.
Treatment Challenges and Emerging Therapeutic Strategies
Treatment of Babesiosis typically involves a combination of antimicrobial agents targeting the parasite. The standard regimen includes atovaquone plus azithromycin or clindamycin plus quinine for more severe cases. Unlike bacterial infections such as Lyme disease, where antibiotics alone suffice, parasitic infections require tailored therapies that address intracellular protozoa.
One significant challenge is the potential for drug resistance and relapse, especially in immunosuppressed patients. Moreover, co-infections with Lyme disease or anaplasmosis may necessitate concurrent treatments with different drug classes, increasing the complexity of management and risk of adverse effects.
Recent research focuses on novel antiparasitic agents and immunomodulatory therapies to enhance host clearance of Babesia parasites. Advances in understanding the parasite’s life cycle and immune evasion mechanisms hold promise for future vaccine development—a critical step given the rising incidence rates linked to environmental changes.
Public Health Implications: Awareness, Prevention, and Future Directions
As awareness of Babesiosis lags behind that of Lyme disease, public health education remains a crucial component in reducing infection rates. Preventative measures mirror those recommended for Lyme disease: avoiding tick-infested areas during peak seasons, using insect repellents containing DEET or permethrin-treated clothing, performing regular tick checks after outdoor activities, and prompt removal of attached ticks.
Surveillance systems need enhancement to accurately track cases of Babesiosis and co-infections with other tick-borne diseases. Improved reporting will help public health authorities allocate resources effectively and guide research priorities.
In conclusion, Babesiosis represents an emerging threat in the landscape of tick-borne illnesses. Its similarities with Lyme disease in transmission but differences in pathogenesis necessitate distinct clinical approaches. Increased awareness among healthcare providers and the public will be essential to mitigate its impact as environmental factors continue to influence vector distribution worldwide.
Notes
- Babesiosis is transmitted by the same tick species responsible for Lyme disease—Ixodes scapularis.
- An estimated 1,000–2,000 cases of Babesiosis are reported annually in the United States but actual numbers are likely higher due to underdiagnosis.
- Co-infection with Lyme disease occurs in approximately 10-20% of patients bitten by infected ticks.
- Babesia parasites infect red blood cells similarly to malaria parasites but are geographically distinct.
- Climate change has contributed to expanding tick habitats into new regions across Europe and North America.